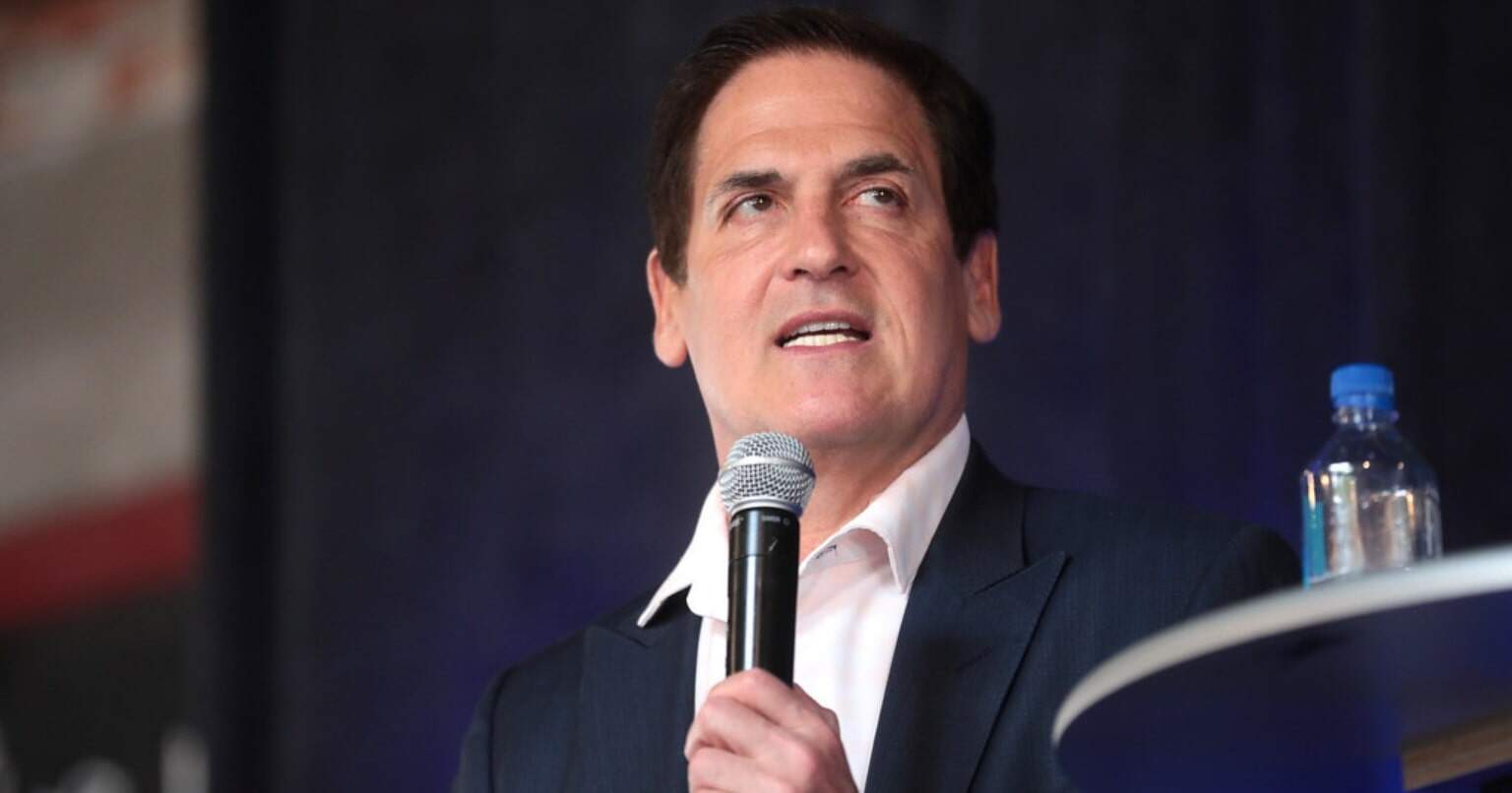
Billionaire entrepreneur Mark Cuban has a simple question that lands like a gut punch for anyone who has ever opened a medical bill. He asked on X why an insurance company would pay $2,500 for an MRI when a center down the street offers the same scan for $350.
He raised that point in mid-January while criticizing how hospitals and large insurers handle prices, and his comments quickly turned into a wider debate about who really benefits from those big numbers.
A viral post that reflects everyday anxiety
If you have ever needed an MRI for a sore knee or a stubborn back injury, you probably know the feeling. The scan itself takes minutes.
The bill can take weeks to arrive and can easily wipe out a big chunk of your savings. National data show an MRI in the United States averages about $1,325, yet the same type of scan can cost as little as roughly $400 or climb well into the five figures depending on the facility and the payer.
People replying to Cuban shared that experience in real time. Some said they were quoted more than $1,500 through insurance, then paid only a few hundred dollars in cash at an independent imaging center.
Cuban took those stories as proof that the system, in his words, rewards high prices instead of protecting patients and employers.
Why the same MRI can cost $350 or $2,500
So what is going on behind the scenes? For the most part, the answer lies in how insurers and health systems negotiate. Research on MRI pricing shows that hospital outpatient departments often charge far more than standalone imaging centers, in part because hospitals layer on facility fees and carry higher overhead.
Those prices are baked into contracts. An insurer might agree to pay a hospital more than $2,000 for a single body-part MRI because that hospital controls the emergency room, trauma care, and many specialists in the area. Walking away from that deal would make the entire health plan look less attractive to employers.
Analysts note that this bargaining power explains a large share of the price gaps seen in brain MRI claims, where systems with more clout tend to command higher commercial rates.
Independent imaging centers have a different reality. They do not run emergency rooms and rarely have the same leverage, so their business lives or dies on patients and referring doctors picking them. That creates pressure to post clearer, lower prices such as $350 or $400 for a standard scan.
GoodRx pricing data and recent industry reviews both point out that hospital based imaging is typically far more expensive than outpatient centers, even within the same city.
Cuban’s bigger target insurers and pharmacy middlemen
Cuban’s frustration is not limited to one MRI bill. In the same series of posts, he argued that the largest pharmacy benefit managers are owned by the biggest insurance companies and serve, in his view, as profit engines.
He warned that if regulators crack down in one area, these giants simply shift their earnings somewhere else and remain, as he put it, too big to care.
That criticism lines up with the model behind his company Cost Plus Drugs, an online pharmacy that buys medications directly from manufacturers and publishes its markups.
The idea is that transparency can undercut opaque pricing games and give patients and employers at least one part of the market where the numbers are easier to understand.
What this means for your premium and your paycheck
It can be tempting to shrug and think that if insurance is paying $2,500 for a scan, it is not really your problem. Health policy analysts repeatedly caution that this comfort is mostly an illusion. Over time, higher medical claims feed directly into higher premiums for employers and workers, larger deductibles, and steeper out-of-pocket limits.
One long-running analysis of medical spending describes healthcare costs as the main driver of insurance prices, which mirrors what many families see when open enrollment rolls around each year.
That is why Cuban’s question hits a nerve. It is not only about a billionaire arguing with insurance executives online. It is about why a parent in a traffic jam on the way to an imaging center worries that a twenty-minute scan might turn into months of payments on a high-interest credit card.
What patients and employers can actually do
There is no quick fix, and experts are careful to say that not every hospital charge is unreasonable.
Yet there are some practical steps that, to a large extent, can tilt the odds in your favor. Consumer guides now encourage patients to ask their doctor if the MRI order can be sent to an independent accredited imaging center, compare self-pay prices with insurance estimates, and confirm whether the facility is in network.
Employers that sponsor their own health plans are also paying attention. Some already steer workers toward lower-cost imaging sites or share tools that list prices for common scans in their area.
Those efforts are still a patchwork, but they show that Cuban is not the only one questioning why a $350 scan turns into a $2,500 claim.
For now, his viral post serves as a simple test for a very complex system. If no one can give a clear, credible answer to that MRI question, it becomes harder to argue that the status quo really serves patients at all.
The official statement was published on X.